
Blüpass is an Ethereum based token that enables multiple users to access our platform designed to better connect
providers, carriers, and consumers. Our platform will put control in the consumers hands to facilitate data
transfers between providers and carriers for electronic health records, claims service, policy and premium
verification, and much more. We believe our blockchain technology supported with smart contracts will
dramatically change the insurance and delivery of healthcare.
Blüpass will revolutionize access to data, healthcare, and the claims process for everyone. We
began our experience by administering benefits in a unique way. Our billing reconciliation
process, HRaspirin, eliminated headaches between HR professionals and carriers. We spent six
years in this space developing strong relationships. As good as our product was, it only solved
for one side of a broken equation. This prompted us to create Blüpass, a total solution.
Blüpass will build a blockchain fabric to connect providers, consumers, and carriers. Historically,
there are three major problems in the healthcare arena. First, healthcare providers must spend
a significant portion of their time and revenue on billing, health records, and treatment
modalities. The provider may not have a complete picture of the consumer’s financial
responsibility or health record. Second, carriers attempt to limit potential fraud through a
lengthy and manual claims process. This process can take up to 6 months in the current
environment to pay claims. Third, consumers are caught in this vortex of uncertainty between
providers and carriers. This turbulence places unnecessary burdens on consumers in the form
of expenses and treatment delays. Blüpass will build a multilayer blockchain to accommodate
existing and new healthcare technologies. We will utilize our unique blockchain ledgers to
deliver instant data for claims service while providing technical support to eliminate fraud for
carriers. Finally, we will build a client centric mobile platform that enables consumers to control
the timing and delivery of medical records and application of claims. Simply put, we believe
consumers should have instant verification of their policy information and claims adjudication
at the point of service. Additionally, a simplified financing system in the U.S. could result in cost
savings exceeding $350 billion annually, nearly 15% of health care spending. Imagine any other
experience in which you buy a service and the provider can’t tell you how much it's going to
cost up front and you are expected to pay whatever bill they send you 6 months later. When
you buy insurance against this uncertainty, the carrier demands to be paid on time without
exception but can't offer claims service at time of service. Blüpass solves for these
inconsistencies.
Executive Summary
Unique to the ICO world is a real company with real products and solutions. Blüpass is a
product born from innovation as we have solved reconciliation headaches for over six years.
Blüpass will change everything that is deficient in the Healthcare industry and transform it into
a consumer centric, egalitarian model. For many years, carriers and providers have worked
tirelessly to reduce overhead due to fraud and problematic HIPAA Privacy and Security
regulations in regards to billing and electronic medical records, all at the detriment to the
consumer claim process and data ownership. By utilizing Blockchain technology to build our
platform, we will transform the way data flows between each simultaneously. We will solve all
three client components at once. Blüpass is a consumer driven platform that solves claims
processing delays, provider overhead, and carrier claims fraud. Insurance claim inaccuracies
alone costs patients and providers up to $600-800 billion annually. Blüpass benefits from the
existing payment structure, HRaspirin. Our payment reconciliation system allows for various
groups, businesses, associations, unions, or individuals to establish traditional individual groups
or group platform benefits and eliminate human resource administration of the benefits plan.
We collect premiums, reconcile invoices automatically, monitor individuals for missed
premiums, and consolidate multiple carrier invoices with our proprietary software. We will use
Blüpass blockchain ledgers to verify premiums instantly against policy information to enable
guarantees on claims. HRaspirin’s success positions Blüpass with enormous options for positive
growth from day one. Blüpass will enhance HRaspirin’s client experience via instant
verification of consumer premiums, policy provisions, and providers universal coding to enable
settlement of specified provisions at the time of service.
Overview of Healthcare Market
Healthcare providers are often torn between the desire to serve their community and
maintain the finances of a tormented business model. Administrative stresses and
pressures force providers to compensate with ever rising price structures.
The United States’ multiple-payer health care system requires substantial
effort and costs for administration, with billing and insurance-related
(BIR) activities comprising a large but incompletely characterized
proportion. A number of studies have quantified BIR costs for specific
health care sectors, using micro-costing techniques. However, variation in
the types of payers, providers, and BIR activities across studies
complicates estimation of system-wide costs. Using a consistent and
comprehensive definition of BIR (including both public and private
payers, all providers, and all types of BIR activities), we synthesized and
updated available micro-costing evidence in order to estimate total and
added BIR costs for the U.S. healthcare system in 2012. BIR costs in the
U.S. healthcare system totaled approximately $471 ($330 – $597) billion
in 2012. This includes $70 ($54 – $76) billion in physician practices, $74
($58 – $94) billion in hospitals, an estimated $94 ($47 – $141) billion in
settings providing other health services and supplies, $198 ($154 – $233)
billion in private insurers, and $35 ($17 – $52) billion in public insurers.
Compared to simplified financing, $375 ($254 – $507) billion, or 80%,
represents the added BIR costs of the current multi-payer system.
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4283267/)
Administrative costs in the United States consumed an estimated $156
billion in 2007, with projections to reach $315 billion by 2018 (Collins et
al., 2009). With the time, costs, and personnel necessary to process
billing and insurance-related (BIR) activities from contracting to payment
validation on the provider side and the needs of payers to process claims
and credential providers, significant redundancy and inefficiency arises
from healthcare administration. Adding to concerns is emerging evidence
of an inverse relationship between administrative complexity and quality
of care (Himmelstein and Woolhandler, 2002). The presenters in this
session approach estimating excess administrative costs from a variety of
macro- and microeconomic levels, all with the goal of identifying the
portion of expenditures spent on administration that could be reduced by increasing the efficiency of the delivery system, which highlights the need
for administrative simplification and harmonization.
Payment Collection
HRaspirin currently solves for consumer premium collection, consolidation,
reconciliation, and remittance. Our unique platform retains the experience of payroll
deducted premiums without the headache to businesses and human resource
departments. We have already achieved milestones in policy persistency unseen before
by carriers resulting in several private label negotiations on HRaspirin’s software. This
existing technology will be enhanced through Blüpass’s blockchain ledgers to provide
needed instant verification of universal billing codes to the policy provisions provided in
policies held by consumers. Blüpass will enable carriers to transfer specific policy claim
provision adjudication to Blüpass for instant pay. Providers using Blüpass will access
instant billing utilizing EHR and our marketplace.
According to a MGMA–Medical Group Management Association report,
physicians will send an average of 3.3 billing statements before a
patient’s outstanding balance is paid in full. The trickiest conversation a
practice has is that of collecting patient balances.
The delay may have multiple causes, such as:
- Practices’ reluctance to talk to patients about money
- Physicians’ refusal to enforce payment policies with longtime patients or those who are going through financial hardships Ineffective patient collection policies, possibly because they’re focused on payer Outdated billing and payment systems
WHY SUPPORT US?
The collaboration between customers, suppliers and safety net providers is cracked in the Healthcare framework.
Industry Know How
Blüpass has the best group of industry experts. They are hone pioneers with years of experience and devoted blockchain specialists with a reputation of fruitful Blockchain ventures
Self Regulation
Blockchain will decentralize the way we store data and oversee data. This will prompt a diminished part for a standout amongst the most critical controllers on the planet, the agent
Convenient Benefit Utility
Blüpass encourages PBU’s that accommodate strategy data, supplier charging and safety net provider guarantees in a split second. The safe Blockchain record is the thing that makes this all conceivable. This innovation drives Healthcare frameworks into what’s to come.
Industry Know How
Blüpass has the best group of industry experts. They are hone pioneers with years of experience and devoted blockchain specialists with a reputation of effective Blockchain ventures
Misrepresentation Prevention
Shoppers will profit by diminished premiums and impetuses. Blüpass’ savvy contracts diminish misfortune because of misrepresentation. Bearer reserve funds can be passed on to purchasers as premium diminishment because of effective cost sparing measures. Buyers will likewise have true serenity their EHR is protected from altering or data fraud.
Adaptability
Protection is a $7 trillion worldwide market. By turning into an early adopter of moment assert benefit, Blüpass can pick up an imperative preferred standpoint.”
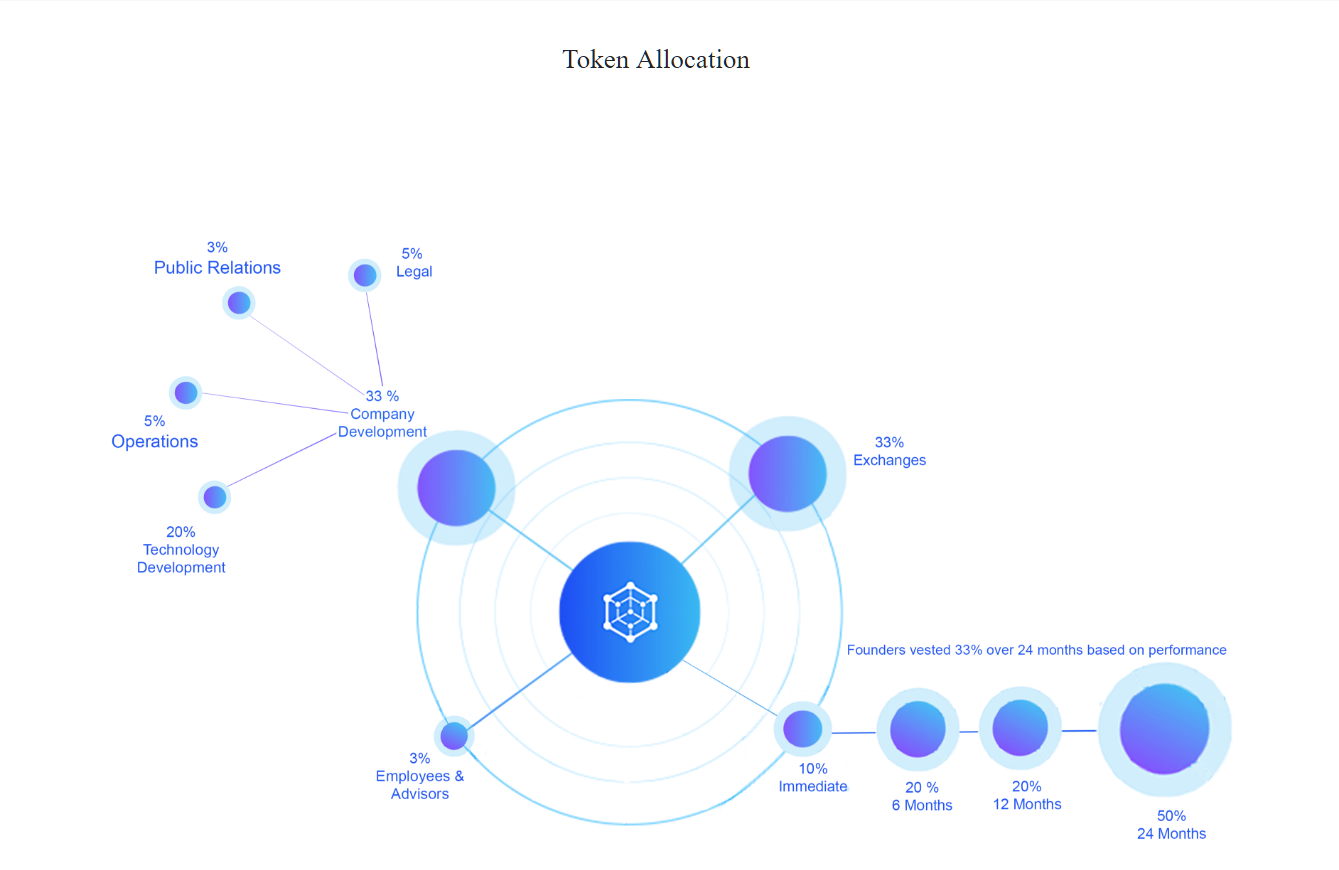
Blüpass generates Token 6 billion (BLU). Consumers outside our network buy tokens (blue) to access our system. The operator – a contract for the purchase of Blues, to facilitate their right to the Blupass system. Onced is used, tokens can be reused. The operator can store your tokens for an unlimited period of time or you will re-sell the system. This worm is not much about the ICO project, is a pre-blue flag blue marker
Token Information
Start
May 15, 2018 (12:00 AM CST)
End
July 15, 2018 (11:59 PM CST)
Acceptable currencies
ETH
Total token supply
6 billion
Soft cap
$3 million
Number of tokens for sale
500 million BLUs, with 150 million released for pre sale and 350 million released for official ICO
Tokens exchange rate
1 ETH per 4000 BLUs
Minimal transaction amount
1 ETH
Token Standard
ERC-20
Hard Cap
$30 million
May 15, 2018 (12:00 AM CST)
End
July 15, 2018 (11:59 PM CST)
Acceptable currencies
ETH
Total token supply
6 billion
Soft cap
$3 million
Number of tokens for sale
500 million BLUs, with 150 million released for pre sale and 350 million released for official ICO
Tokens exchange rate
1 ETH per 4000 BLUs
Minimal transaction amount
1 ETH
Token Standard
ERC-20
Hard Cap
$30 million
ROAD MAP

.

MORE INFORMATION :
No comments:
Post a Comment